There are a variety of paths to practicing medicine, and an alternative route to the MD (Doctor of Medicine) degree offered by traditional allopathic medical schools is the DO (Doctor of Osteopathic) degree offered by osteopathic medical schools. Over recent years, there has been a boom in the number of osteopathic schools and graduates; at present, more than 25% of U.S. medical students attend DO schools. This increase has been largely stimulated by the shortage of primary care physicians in the U.S., which could be as high as 48,000 primary care doctors and 77,100 specialists by 2034, primarily due to population growth and aging. Many DO programs also have an added mission of providing doctors to underserved populations (poorer neighborhoods and towns that have doctor shortages).
There are a variety of paths to practicing medicine, and an alternative route to the MD (Doctor of Medicine) degree offered by traditional allopathic medical schools is the DO (Doctor of Osteopathic) degree offered by osteopathic medical schools. Over recent years, there has been a boom in the number of osteopathic schools and graduates; at present, more than 25% of U.S. medical students attend DO schools. This increase has been largely stimulated by the shortage of primary care physicians in the U.S., which could be as high as 48,000 primary care doctors and 77,100 specialists by 2034, primarily due to population growth and aging. Many DO programs also have an added mission of providing doctors to underserved populations (poorer neighborhoods and towns that have doctor shortages).
Contact us a for a free medical school admissions consultation!
A principal difference in the two approaches is that MD programs offer the traditional approach of Western medicine, whereas the DO philosophy is more holistic, aiming to treat each patient as a whole person, rather than a compilation of symptoms or injuries. The DO approach acknowledges that all of the body’s systems are interconnected, that the body has the capacity to heal itself, and that the musculoskeletal system is especially important in reflecting and affecting the condition of all other systems. As the Philadelphia College of Osteopathic Medicine states on its website, “DOs are trained to be doctors first, and specialists second.”
DO doctors practice primary care to a greater degree than MDs, including the specialties of internal medicine, family medicine and pediatrics, and help fill physician shortages in these fields. Close to 60% of DO-trained physicians enter primary care, compared to 26% of MD graduates.
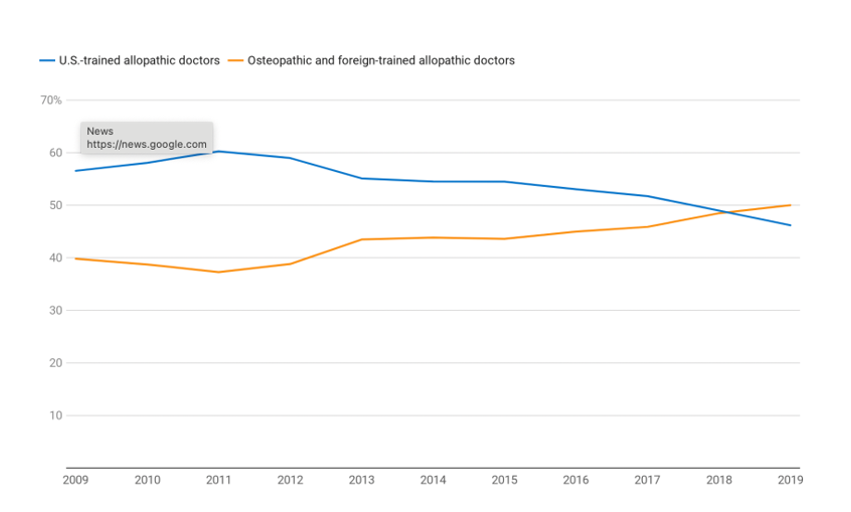
In fact, the percentage of US-trained allopathic doctors who seek a residency in primary care has been declining, while the percentage of osteopathic and foreign-trained allopathic doctors has been rising. In 2018, the percentage was equivalent, at about 48%, while 2019 was the first year in which the percentage of osteopathic and foreign-trained doctors interested in primary care exceeded that of US-trained allopathic doctors, as shown in the graph below.
Percentage of Doctors Interested in Primary Care, by Type of Training
How are DO and MD Doctors Similar?
- Attend 4-year medical school
- Complete specialty training through internships, residencies, and fellowships
- Require licenses from state medical specialty boards to practice
- Can practice in all 50 states in any specialty and provide all medical services
- May prescribe medications as appropriate
How are Osteopathic Students Unique?
- Trained to focus on the whole person, and consider lifestyle, environment, and psychological factors in treatment.
- Required to take up to 500 hours of additional classwork on osteopathic principles and aligning the musculoskeletal system.
- Learn the approach of Osteopathic Manipulative Treatment (OMT), also called Osteopathic Manipulative Medicine (OMM), which involves applying gentle pressure with the hands to diagnose, treat, and prevent illness or injury.
- Required to take the Comprehensive Medical Licensing Exam (COMLEX), whereas MD students must take the United States Medical Licensing Exam (USMLE) to practice. As a side note, DOs may also opt to take the USMLE exam to expand their options for residencies.
According to Steve Toplan, Director of Admissions at Touro College of Osteopathic Medicine, “The biggest difference [between MD and DO programs] is the fact that in the OM realm, students are taught osteopathic muscle manipulation. Other than that, the medical school curriculum is virtually the same.”
Interestingly, while OMM is the big differentiator between MD and DO training, “only 5% of DOs use hands-on techniques; mostly it’s in their heads in terms of the philosophy of how the body fully integrates,” said Brooke Birdsong, former Associate Director of Admissions at Kansas City University’s College of Osteopathic Medicine.
Why Pursue a DO Degree?
There are several reasons why students may choose to pursue a DO degree.
Some students may feel that the holistic philosophy is more aligned with their values regarding medical care. Dr. Jennifer Caudle, DO and Associate Professor at Rowan University School of Osteopathic Medicine, says that she was drawn to its “mind-body-spirit whole-body approach to medicine.” In addition, she felt that historically DO schools were more open to non-traditional applicants, as well as a more diverse pool, noting that “DOs were some of the earliest institutions that accepted women and people of color.” Currently, 43% of practicing DOs are women.
Others are drawn to the “hands-on” osteopathic manipulation approach. David Abend, DO, has over 25 years of clinical private practice experience. He began in primary care and now exclusively practices OMM because “I enjoy using my hands.” He is one of a small number of DOs trained and Board-Certified in OMT and Osteopathic Craniosacral Manipulative Medicine (OCMM), also known as cranial osteopathy.
Finally, DO programs are typically less selective than MD programs, so students who are not as competitive a candidate for MD admissions in terms of GPA and MCAT scores or extracurricular activities may benefit from the higher admit rate of most DO programs. In 2020, the mean MCAT score for DO matriculants was 504.31 and their mean GPA was 3.54; for MD matriculants, these scores were 511.5 and 3.73, respectively. (In 2022, MD scores were even higher, at 511.9 and 3.75; such recent data is not yet available for DO matriculants.)
Ben Kramer, a graduate of the New York Institute of Technology College of Osteopathic Medicine, was always motivated to become a doctor, but did not realize how important it was to pursue medically-related activities during college, such as research, in order to be a competitive MD applicant. He spent the year after college as a scribe in the Emergency Department of a hospital, which provided patient contact and shadowing. He is now practicing at the Cleveland Clinic.
What is the Availability of DO Medical Colleges?
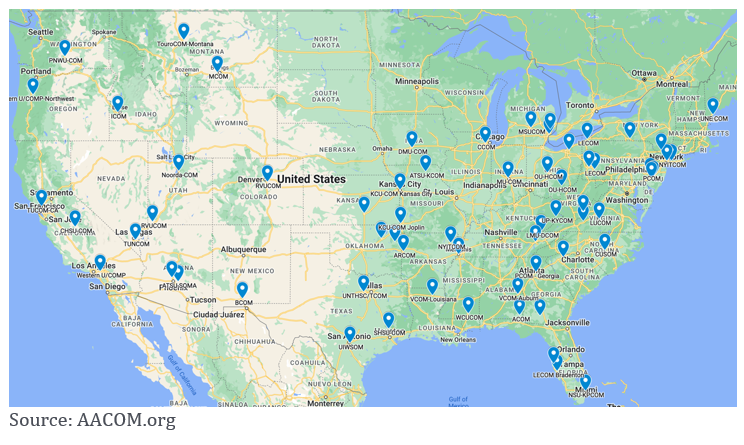
There has been a significant increase in the number of osteopathic medical colleges (from 5 in 1968 to 37 in 2022), as well as the number of osteopathic graduates (from 971 in 1978 to more than 7,000 at present). In spite of this dramatic increase, most med schools and med school graduates are still affiliated with MD programs. As of 2021 there were 155 MD schools with preliminary, provisional, or full LCME accreditation and, as of 2022, 21,051 MD graduates. For example, New York State has three osteopathic medical colleges—New York Institute of Technology, Touro, and Lake Erie—compared with 15 allopathic medical schools, including Columbia, NYU, and Weill Cornell. (See this map of osteopathic schools across the United States.)
Changes in Residency Matching
After graduating from medical school (either with an MD or DO degree), the next step in medical education is to participate in a residency program to obtain clinical experience. The process of applying for a spot occurs through a “matching” system in which students and programs rank each other and are then matched by an algorithm. Up until recently, there were two separate processes for MDs and DOs. However, in June 2020, the Accreditation Council for Graduate Medical Education (ACGME), American Osteopathic Association (AOA), and American Association of Colleges of Osteopathic Medicine (AACOM) announced a transition to a single graduate medical education accreditation system that integrates all allopathic and osteopathic residencies.
The participation of DO students in the NRMP residency match program has grown substantially alongside this transition. In 2022, 7,303 U.S. DO seniors submitted rank order lists of programs, 202 more than in 2021 and an all-time high. 6,664 of these matched to PGY-1 positions, a match rate of 91.3 percent, up 2.2 percentage points from the previous year.
Which Path is Best for You?
It all depends! If you are passionate about primary care and think the whole-person osteopathic approach to medicine could be an asset to your education, a DO program could be the right fit for you.
According to Alan Stricoff, DO, FACP, Senior Medical Director at Cigna and Chief Medical Officer of Cigna’s client-focused onsite health and coaching business,
“If you want to become a highly competitive specialist, like an ophthalmologist, dermatologist, or specialty surgeon, the path is easier from a good MD program. However, if you are interested in primary care, there is no difference, and you may even be better off coming from a DO program, because of the focus on primary care.”
Navigating the many tracks to medical school can be daunting, but here at Collegiate Gateway, we are happy to help you in finding the best path to reaching your goals. Feel free to contact us!